In the midst of the Covid-19 pandemic, everyone is trying to figure out how to make the built environment safer and more healthful. Heating, ventilation and air conditioning (HVAC) systems affect communicable disease by reducing the concentration of infectious particles in the air, thus reducing the risk of infection.
The most common method to reduce indoor virus and bacterial pathogens is through dilution by introduction of outdoor air ventilation and associated exhaust. However, this may pose challenges because of the limitations of existing heating and cooling equipment and existing ductwork, as well as operational costs associated with increased energy use to heat, cool, and dehumidify outdoor air.
Air filters
Air filtration or HVAC air treatment technologies work to either capture and remove pathogenic particles or to deactivate a pathogen’s ability to infect living cells, effectively rendering it inert.
Air filters, though effective at removing large particulates such as dust, struggle to capture smaller particles and require commensurately denser filter material weave to capture small particles. Viruses such as the Sars-Cov2 (Covid-19) virus are very small, just over 0.1 microns, and many common HVAC filters (MERV 6-8 efficiency) are able to capture less 10% of the viral load in the air passed through them. High-efficiency HEPA filters are able to capture much more of the viral load, more than 99%, but are expensive to replace and require HVAC systems that are specifically designed for them and have enough fan energy to push the air through the very dense material of a HEPA filer.
Importance of humidity
In the past, humidity control has been considered a comfort issue. In the summer, air conditioning systems help most buildings control humidity reasonably well. But in the winter, for many climates, unless the building can add moisture to the air, the humidity levels can get very low.
Recent research is showing that low humidity levels can increase the likelihood of infection in several ways. First, many of the bacteria, viruses and other pathogens that lead to infectious diseases tend to survive and grow best in very high and very low humidity levels. Maintaining the indoor humidity level between 40 and 60 percent reduces the number of pathogens able to survive and subsequently cause infections.
Studies performed by Harvard Medical School have shown that low relative indoor humidity is strongly associated with higher infection rates. One of the first lines of defense against respiratory infections is the lungs’ respiratory mucous barrier, the surface liquid layer. The cilia of the lungs capture and remove invading pathogens and particles before they can penetrate deeper into the lungs. As ambient humidity levels decrease, so does the ability of the lungs’ mucous layer to help prevent infection.
A team at the Mayo Clinic humidified half of the classrooms in a preschool and left the other half alone over three months during the winter. Influenza-related absenteeism in the humidified classrooms was two-thirds lower than in the standard classrooms. Because winter humidification was mostly looked at as a comfort nicety, it often was excluded from building systems. Humidifiers require regular maintenance and even when employed in the design, they are frequently abandoned over time because of failure. Controlling humidity may be one of the best measures that can help prevent infections.
SIDEBAR: Three approaches
With so much research and several options it may be difficult for facility managers to decide what is best for their built environment. Here are three major options.
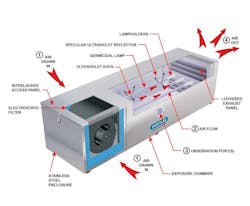
• UV-C Lighting: The efficacy of ultraviolet germicidal radiation UV-C lights have been proven to effectively kill pathogens by destroying its DNA/RNA, thus eliminating its ability to replicate. The deactivation effectiveness is a function of exposure time and intensity of the ultraviolet light. The nature of the technology requires the pathogen be in line of sight to “see” the UV-C bulb, thus air must be circulated from the space to be treated by UV-C lights within the HVAC system.
Care must be exercised because direct exposure to ultraviolet light is harmful to human skin and eyes, and also may deteriorate many building materials.
• Dry hydrogen peroxide: Hydrogen peroxide has long been used for room disinfection in gaseous fog systems. However, the liquid hydrogen peroxide in these systems is used at concentrations well beyond typical safe levels for occupied spaces (up to 750 PPM). Dry Hydrogen Peroxide (DHP) technology was developed in the biodefense industry and shows significant effectiveness at reducing bacteria, mold, and viruses.
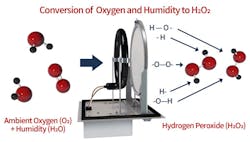
The system produces DHP from the ambient humidity and oxygen naturally present in the air, through the use of a catalyst activated by a specific-wavelength ultra-violet light. The technology creates a safe level of hydrogen peroxide gas, around 0.025 PPM, which reduces unwanted microbial contamination in the air and on surfaces.
Human lungs naturally produce hydrogen peroxide in concentrations around 1.8 PPM, and the OSHA standard for safe hydrogen peroxide exposure is 1 PPM in 24 hours. Because DHP is a gas rather than an aerosolized liquid, it can reach all areas of a space. All microorganisms require water from the environment to survive. Because of the similarity of the hydrogen peroxide molecule (H2O2) to water (H2O), it can attach itself to a microbe’s access points. Once attached, a natural breakdown of the microbe occurs.
• Bipolar Ionization: Ions are positively or negatively charged oxygen atoms that are present naturally in the air and are found in the highest concentrations at high elevations, at the ocean shore or after thunderstorms. Bipolar ionization or needle-point bipolar ionization technology artificially generates positive and negative ions that are released into the airstream or space.
This accomplishes three things:
--Kills the Virus
The ions produced are attracted to pathogens such as viruses and bacteria. These ions steal away hydrogen atoms from the pathogens, leaving them to die. In viruses including the SARS-Cov-2 virus that causes Covid-19, the charged ions bind to the cellular receptors that enable the virus to attach to and infect human cells, rendering the virus particle inactive and non-infectious, effectively “killing” the virus. Infected occupants will contribute to the pathogen load over time as they breathe or cough. However, ions are continually added to the space and function to reduce the concentration of infectious pathogens over time.
--Captures Particles
The ions cause particles that are suspended in the air to become either positively or negatively charged. They are then attracted to each other, effectively increasing their mass and size. As the particles agglomerate (stick together), they create a larger surface and mass that can then fall to the floor or travel within the airstream back to filters in the HVAC system, which can now remove the agglomerated particles from the airstream more effectively. This agglomeration reduces airborne particles (i.e., dust, pet dander, pollen). The air filtration system easily captures the larger particles, significantly increasing the capture efficiency of HVAC filters and PPE masks and respirators.
--Breaks Down VOCs
Odors and volatile organic compounds (VOCs) are broken down by the bipolar ions, resulting in the accelerated elimination or reduction of odors. Ions react with VOCs to break them down into constituent components that are naturally occurring within the atmosphere.
Studies completed by researchers independent of ionization manufacturers have shown statistically significant health benefits to occupants residing in ionized spaces in real world applications. For example, results have shown a 70% reduction in headaches and 60.3% reduction in flu-like symptoms.
McNutt, PE, is a Senior Associate at SFCS and oversees its engineering department. He has more than 10 years of experience in development, design and integration of mechanical systems. He brings extensive higher education design experience as well as a degree in chemical engineering.
About the Author
Allen McNutt
Senior Associate
Allen McNutt, PE, is a Senior Associate at SFCS and oversees its engineering department. He has more than 10 years of experience in development, design and integration of mechanical systems. He brings extensive higher education design experience as well as a degree in chemical engineering.